This page provides information to help you understand the process of having a hip joint replacement (arthroplasty). It is a guide – your care may vary depending on your individual needs. Please read this information before your surgery.
If you have any questions, please ask your Orthopaedic Consultant, Registrar, Doctors, Nurses, or Therapists.
In this section:
Hip Replacement Operation Potential Risks and Complications Expected and Potential Outcomes Arthroplasty Service & Appointments Nursing Care and Recovery Pharmacy and Medicines Physiotherapy Occupational Therapy Going Home & Transport Dressing Aids Useful Information & Contacts
Hip Replacement Operation
The hip joint is a ball-and-socket joint. The head of your thigh bone (femur) forms the ball, which fits into a cup-shaped socket (acetabulum) in your pelvis. Over time, or due to arthritis or injury, this joint can become painful, stiff, and difficult to use.
In a hip replacement, the worn-out joint surfaces are removed and replaced with an artificial joint (prosthesis). This reduces pain, improves mobility, and makes day-to-day activities such as walking, bending, and dressing easier.
The main reasons for having the operation are:
- Pain in your hip that affects your daily life
- Difficulty walking or climbing stairs
- Stiffness that makes it hard to move the joint
- Loss of independence due to hip problems
This is major surgery that will take approximately 45 minutes to one and a half hours. Added to this will be the time you spend in the anaesthetic area before surgery and in the recovery area after surgery until you are stable enough for transfer to the orthopaedic ward. You should plan to go home from hospital in 1-2 days after your admission.
While most joint replacement operations take place without complications all operations do carry some risk and the potential for complications. These include infection, dislocation, blood clots, and swollen limbs and delayed wound healing. It carries a tiny risk of death.
Potential Risks and Complications
Hip replacement is a common and successful procedure, but like all major operations it carries some risks.
- A small number of patients develop wound or deep joint infection.
- Signs include redness, warmth, wound discharge, or a temperature over 38°C.
- Rarely, infection may occur months or years later.
- If infection develops, further surgery and antibiotics may be required.
- A deep vein thrombosis (DVT) is a clot in the leg veins. It can cause swelling, heat, and pain.
- A pulmonary embolism (PE) is when a clot travels to the lungs, which can be life-threatening. Symptoms include sudden breathlessness, chest pain, or fainting.
- You will be given blood-thinning medication and advised on exercises to help prevent clots.
- The artificial hip can dislocate in the first 12 weeks.
- Signs include sudden pain, the leg turning outwards, and difficulty moving the leg.
- Following hip precautions will reduce the risk.
- Leg length difference (sometimes unavoidable)
- Nerve damage (rare, usually temporary)
- Numbness or altered sensation around the scar
- Swelling, bruising, and pain that may last weeks to months
- Prosthesis loosening after many years, sometimes requiring revision surgery
- A small risk of serious complications such as heart attack, stroke, or death (approximately 0.1%)
Expected and Potential Outcomes
During your stay in hospital you will be part of the ‘Enhanced Recovery After Surgery’ (ERAS) programme. The term enhanced recovery is used to describe an approach to performing joint replacement surgery and promoting recovery. The evidence shows that the approach taken delivers better outcomes and a better experience of care for patients requiring surgery.
Occasionally slight numbness around the scar or part of the leg can happen but this is not anything to worry about.
Swelling of the foot and ankle is very common after surgery and may last several months. The swelling is usually better first thing in the morning and gradually increases as the day progresses. Doing your ‘circulatory exercises’ will help and having a one hour rest on the bed in the afternoons should help reduce swelling.
You can expect pain for 6-12 weeks after surgery. The pain may be referred into the knee and shin. It is not unusual to have pain in other joints as your gait may be altered in the first period after surgery.
It is common to become constipated after surgery. This can be due to several reasons including the effects of analgesia (painkillers), fasting and change of mobility. Please speak to staff if you become uncomfortable.
Sometimes patients will lose blood through surgery. If this happens you may require a blood transfusion. Like all medical interventions, a transfusion will only be offered if really necessary.
Arthroplasty Service & Appointments
The Arthroplasty Service is nurse-led and provides support before and after your surgery.
- Available Monday to Friday, 8am – 5pm
- You can call and leave a message; calls will be returned as soon as possible
- You will attend an Arthroplasty Education Group before your surgery, which lasts about an hour and prepares you for what to expect
- A follow-up clinic appointment is arranged for 6 weeks after your operation to check your wound, movement, and walking progress
Nursing Care and Hospital Recovery
- You will go to the recovery area before returning to the ward.
- You may have monitoring equipment, a drip, or oxygen in place.
- You may be helped out of bed the same day as your operation with staff support.
- Most people are ready to go home after 1–2 days.
- Tell staff if you are in pain; medicines can be adjusted.
- Take painkillers before physiotherapy or walking sessions.
- Tablets are usually used instead of injections once pain is under control.
- You’ll be given blood-thinning tablets during your hospital stay and after you go home (usually for 35 days).
- Do your ankle and leg exercises regularly.
- Watch for any unusual bleeding and report it immediately.
- Your dressing is designed to stay in place for up to 2 weeks.
- Clips are removed by a district nurse at around 12–14 days after surgery, unless dissolvable stitches are used.
- Special dressings with a small battery pack may be used; the battery lasts 5–7 days.
- Constipation is common; drink fluids, eat fruit and vegetables, and let staff know if your bowels don’t move for 2 days.
- Medicines can be given for constipation or sickness if needed.
Pharmacy and Medicines
Please bring an adequate supply of your medicines into hospital when you attend the pre-admission clinic and when you attend for surgery. This will ensure the healthcare team can determine what medicines you normally take and your medicines are available on the ward.
Your regular medicines will continue where appropriate and you are likely to be given some medicines to relieve pain, prevent infection, prevent blood clots, or to treat nausea or constipation.
Knee surgery increases the risk of blood clots. To reduce this, you may be prescribed a short course of blood-thinning tablets (such as rivaroxaban) or injections. These must be taken exactly as prescribed.
Seek medical help if you notice:
- Calf pain or swelling
- Chest pain or sudden breathlessness
- Unusual bleeding (e.g. blood in urine/stool, nosebleeds lasting >5 mins, coughing blood, heavy cuts that won’t stop bleeding)
Rivaroxaban tips:
- Take with food
- Don’t double up if you miss a dose
- Inform your GP if you feel dizzy, faint, or notice side effects
- Tell your doctor about any other medicines, as some increase bleeding risk
You may be prescribed a short course of antibiotic injections around the time of surgery to prevent infection. Occasionally you may require a longer courseof antibiotics if you develop an infection following surgery. Again it is important to complete the course even if you feel well as this will help prevent joint infections. Side effects of antibiotics may include rash or diarrhoea. You should inform healthcare staff if your side effects are troublesome. Please also advise staff if you are allergic to penicillin, for example.
An important part of your care is to ensure that you do not experience excessive pain. A range of painkilling medications are used. Most patients will receive paracetamol, which is a very effective and safe painkiller on its own or in combination with other painkillers. You are advised to take these on a regular basis until the pain is negligible.
You are also likely to be prescribed a stronger opiate painkiller according to your requirements. Opiate painkillers include codeine, dihydrocodeine, tramadol, morphine and oxycodone. These may be given regularly or when you need them in either tablet or liquid form. Other painkillers are sometimes added if you have inflammation or nerve pain.
It is particularly important to take adequate pain relief before movement and physiotherapy. Your painkillers will be rationalised as your pain improves. If you are in pain, please do not suffer in silence and ask your nurse for assistance.
Side effects you may experience with the stronger (opiate) painkillers include drowsiness, nausea and constipation. These side effects can be managed with other medicines or by taking the painkillers at a lower dose or only when needed.
It is common for many surgical patients to become constipated in hospital. The reasons for this include: the effects of surgery, fasting before surgery, change of diet, effects of painkillers and through lack of fluids and reduced physical activity. There is therefore no reason to worry if your bowels do not move as often as normal, but do advise staff if you feel uncomfortable and would like laxatives to help. These can usually be stopped within days when your bowel function returns to normal.
You may feel nausea (sickness) or actually vomit after your operation. In this case you can be offered anti-sickness medicines and your painkillers may be reviewed.
Your pharmacist, doctor or nurse can offer advice and help you with a range of potential medication problems and to respond to any other symptoms that may trouble you.
When You Go Home
Your doctor or nurse will arrange any medicines you need to take home. This process can take a few hours. You’ll usually receive a week’s supply of painkillers and your full course of blood-thinning tablets. Contact your GP if you need more.
Most people have no issues with side effects, but it’s important to take all medicines as prescribed to aid recovery and prevent complications.
Physiotherapy: exercises, walking & stairs
You will receive physiotherapy as part of your rehabilitation while you are in hospital, and occasionally as an out-patient once you are discharged home if appropriate. Physiotherapy will start the same day as surgery.
Before your operation
You can practice your physiotherapy exercises before your operation providing it is comfortable to do so. You should stop any exercise that increases your pain. If you find the exercises difficult then try increasing the repetitions more gradually.
After your operation
The rehabilitation process begins immediately after your operation. This is just as important as the operation itself, and will involve a lot of hard work. All members of the ward team will be involved to help you gain your full potential. We will assist you with the exercises outlined in this booklet and ensure that you are able to walk safely and well. The Physiotherapist will see you normally once a day. You will be expected to then perform your exercises a further 2-3 times in the day. Please note that when you are finished with the walking/mobility aids you should return them to one of the establish centres. Information is found at the back of the booklet or on line. Please do not bring equipment into the hospital or GP practices for returning.
Your hip and leg may be quite swollen after the operation for up to 6-12 weeks.
Because you have had an anaesthetic and are not as active as normal, it is important that you perform some deep breathing exercises to help keep your lungs clear.
- Take a deep breath in through your nose until you feel that your lungs are full of air, hold for a second then sigh the air out through your mouth. Keep your shoulders relaxed.
Perform this exercise 3 times every hour while you are awake.
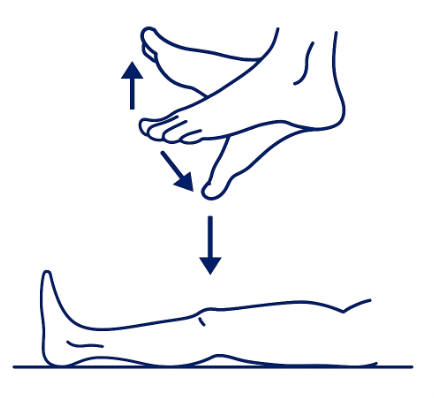
These exercises will improve your circulation while you are immobilised in bed. This will reduce the risk of developing a blood clot.
Point your toes down towards the end of the bed and then pull them up towards you as far as you can. You should feel your skin and calf muscles tightening as you do these exercises.
Pull your foot up towards you, then push the back of your knee down onto the bed. You should feel your kneecap tightening. Hold for 5 seconds, then relax.
Tighten your buttocks together as firmly as you can. Hold for 5 seconds, then relax.
Perform 20 of each exercise every hour while you are awake.
Movement Exercises
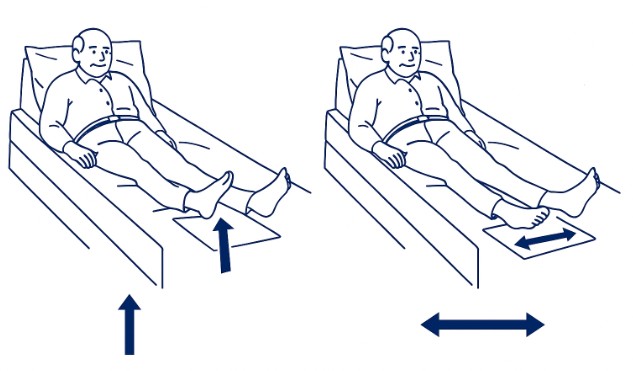
Exercises will usually start under the physiotherapist’s instruction. The exercises are performed initially on a sliding sheet to minimise resistance.
Eventually, you will manage them without this. Sliding sheets are not provided for your discharge home but use a polythene bag.
Your physiotherapist will show you those exercises which are appropriate for you as an individual.
The exercises are usually:
- Pushing the foot up and down slowly and pumping calf muscles.
- Clenching the thigh muscles by pushing your knee onto the bed and tightening the knee cap.
- Bending the knee up towards the chest – not over a 90 degree angle.
- Taking the leg out to the side, keeping the leg straight and back in to the mid-line but not past the mid-line.
- Hip hitching. This is, in effect, making the leg shorter and longer by tightening the buttocks and the leg muscles.
These exercises should be repeated up to 15 times.
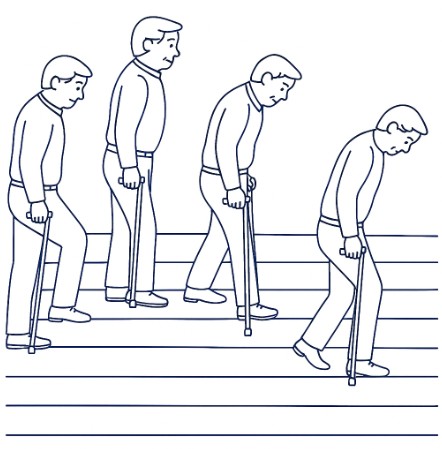
You will begin walking on the same day as surgery with the Physiotherapist and/or Nurse (if medically well enough) with a walking frame to ease the weight on your new hip.
The sequence is always:
- walking aid → operated leg → unoperated leg.
Turning round can be to either side, but you must prevent twisting or pivoting on your new hip. Therefore, feet must be picked up at each step so that the operated leg is not placed too far in or out.
As your confidence and leg control improves, you will progress to walking with crutches/sticks. You should practice with these until a satisfactory walking pattern is achieved.
Most people will manage with two walking sticks by the time the hospital discharge occurs, unless there are associated problems with other joints. Your physiotherapist will assess these problems with you.
It is important that you are measured correctly by your physiotherapist for the walking aid that you are using.
Returning to a “normal” walking pattern is extremely important. Often because of pain and deformity in the affected hip, you have had to change the way you move. This will vary from patient to patient.
It will take considerable time and effort to regain a “normal” walking pattern, but it will get better if you persevere.
Your physiotherapist will help and instruct you in the best way to correct both walking and posture, thus enabling you to use your “new” hip to its full advantage.
You will be taught to negotiate steps and stairs by your Physiotherapist before discharge – always using aids to support the operated leg.
The sequence is as follows:
- Going up: unoperated leg first → operated leg → sticks/crutches.
- Going down: sticks/crutches first → operated leg → unoperated leg.
The physiotherapist will practice stairs with you before you go home.
Occupational Therapy & Hip Precautions
The aim of Occupational Therapy (OT) is to enable you to be as independent as possible with everyday activities after your surgery.
Why am I having Occupational Therapy?
Occupational Therapy is part of your rehabilitation. The Occupational Therapist will talk to you about any difficulties you may have with daily tasks and help you find safe ways to remain independent while following the hip precautions.
What does the treatment involve?
While in hospital, the Occupational Therapist will assess how safely and independently you can manage activities such as:
- Personal activities of daily living
- Domestic tasks
- Leisure activities
Because of the risk of dislocation, you should not sit on low beds, chairs, or toilets. Before your admission, you will be asked to complete a measurement form so that appropriate equipment can be delivered to your home before surgery.
The Four Basic Hip Precautions
These precautions help prevent dislocation. They must be followed for at least 12 weeks after your operation (and ideally long term):
- Do not cross your legs – always keep your operated leg slightly out to the side, away from the midline of your body.
- Do not bend your hip past 90 degrees – avoid bending forward while sitting or lifting your knee too high.
- Do not twist your operated leg inwards – when walking or turning, always keep your toes and kneecap pointing straight ahead.
- Do not roll or lie on your unoperated side – for the first 6 weeks it’s best to avoid lying on either side unless assisted by nursing staff. After 6 weeks, you may lie on your operated side, though it may feel uncomfortable. If you lie on your unoperated side, always place a pillow between your legs for support.
From 12 weeks onwards, you can gradually return to whichever sleeping positions you find most comfortable.
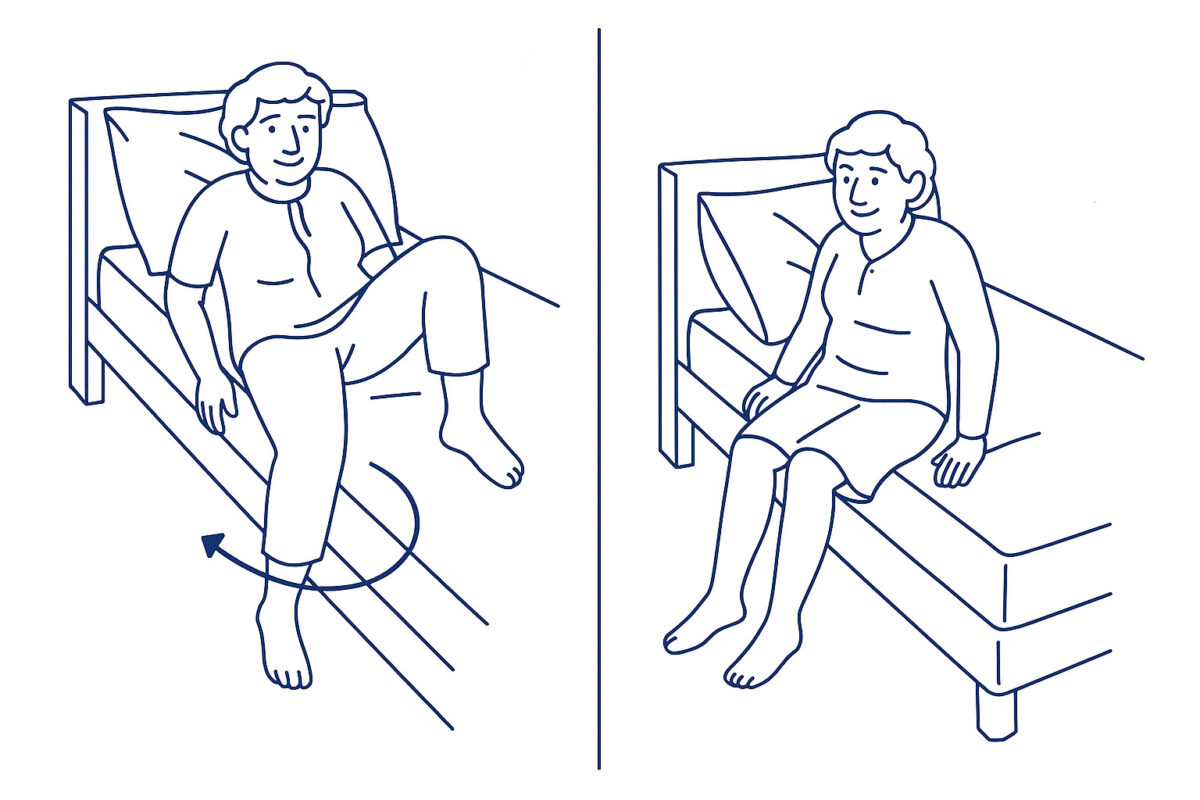
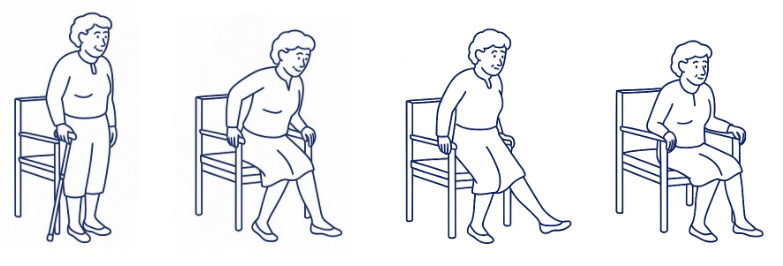
- Sit up in bed and gently pivot your bottom while lifting your legs out one at a time. Keep your trunk and operated leg in line, avoiding bending past 90 degrees.
- Sit upright with both feet flat on the floor.
- Place your hands on the bed beside you, push down, and stand up while drawing your operated leg slightly back.
- Once standing and balanced, take hold of your walking aids.
Getting back into bed is the reverse process. Always support your operated leg and pivot carefully.
- Baths: Do not attempt to get in or out of a bath for 12 weeks after surgery.
- Showering in a bath: Avoid stepping into a bath to shower until you no longer need to follow hip precautions.
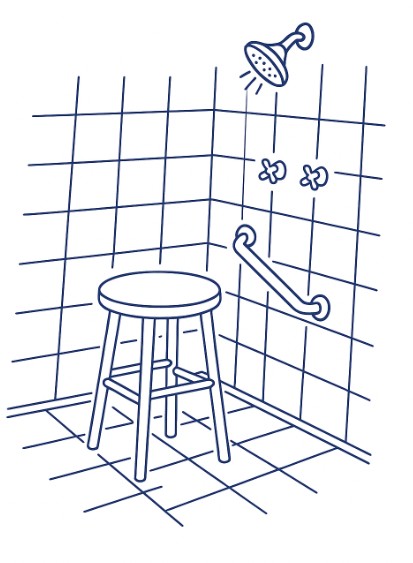
- Showering in a cubicle: A high shower stool may be used. Wash your legs and feet using a long-handled sponge or brush. To step out, place weight on your unoperated leg first, then carefully bring out your operated leg.
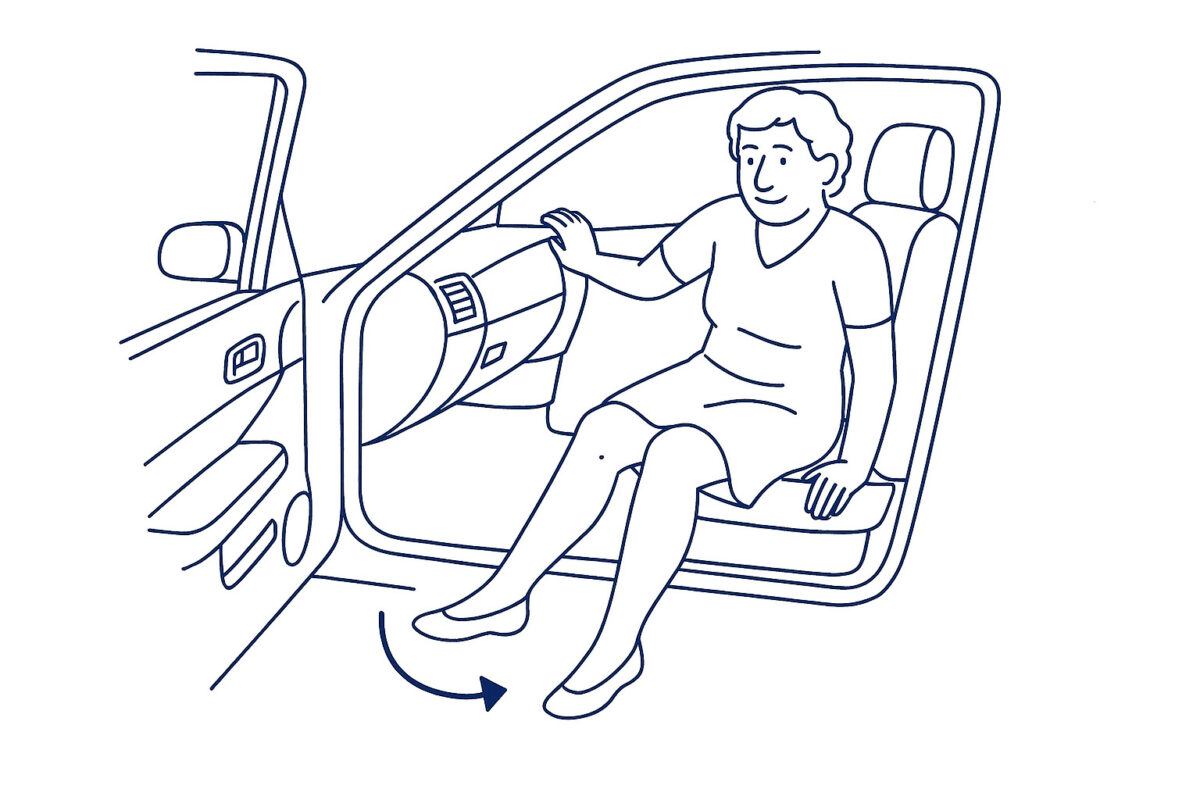
When getting into a car, make sure the passenger seat is as far back as possible and slightly reclined. Back up to the seat until the backs of your legs touch it, then sit down carefully while keeping your operated leg straight out in front. Once seated, pivot your bottom and bring both legs into the car together. To get out, reverse this process – swing both legs out first, then stand up carefully using your arms for support.
- Always follow the hip precautions.
- Avoid standing for long periods – a perching stool may help.
- Spread household chores evenly through the week.
- Rest regularly.
- Avoid heavy activities (like vacuuming) for at least 6 weeks. Ask friends or family for help in the short term.
You can usually cook as before, but do not lift hot dishes from the oven as this requires both hands. Instead, use the hob, grill, or microwave for the first 4 weeks.
- Always use your sticks (or one stick and the work surface) when moving around.
- You may stand without sticks when working at the sink, table, or cooker.
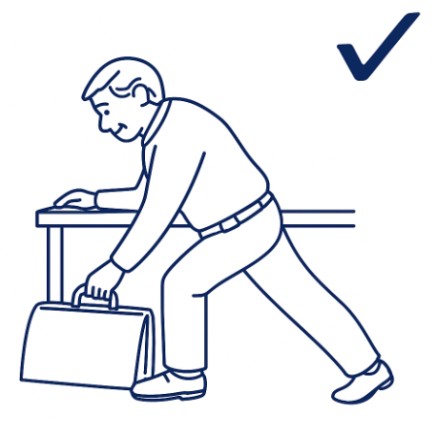
- Avoid bending — instead, hold onto something solid and slide your operated leg behind you, keeping it straight while bending your unoperated knee.
Activities such as gardening, dancing, bowling and golfing may be recommenced 12 weeks after your operation. Initially activities should be undertaken gently and without excessive effort. Always pay attention to your hip. If you experience an increase in pain you should ease back on the effort of the activity or stop and try again later in your recovery.
Low impact activities such as walking can start immediately after surgery by gradually increasing this activity to your pace of recovery. Exercise bike is usually safe to start 12 weeks after your surgery when it is comfortable to climb on and off the bike.
Swimming is a good form of low impact exercise. However, you should wait until you have had your 6 week post-surgery review to ensure that your wound is well enough healed to go back into the water. Breast stroke is allowed 12 weeks after surgery but only if it is comfortable to do so. If you experience discomfort or pain with this stroke you should stop and change the type of stroke. Resistance walking in the swimming pool is allowed.
Going Home & Transport
After a hip joint replacement you should plan to be going home in 1-2 days after your admission.
Various members of the multidisciplinary team liaise with each other to ensure that you have a safe and effective discharge home.
Discharge planning commences at the pre-operative assessment clinic and continues during your stay on the ward.
Please note you can be discharged at weekends.
Do:
- Take short, regular walks
- Continue physiotherapy exercises 3–4 times a day
- Use walking sticks as advised
- Lie flat on your back for an hour each day
Do not:
- Bend past 90° or twist your operated leg
- Cross your legs or kneel
- Sit in low chairs or lean forward too far
- Travel long distances
- Drive until at least after your six week appointment
While there is no need to advise DVLA you are advised to inform your insurance company that you have had surgery.
Once you are 12 weeks following your hip replacement you can begin the process of slowly returning to normal activities. You may begin the process
of stopping the use of your OT equipment. Please note that when you are finished with the OT aids you should return them to one of the establish centres. Information is found at the back of the booklet or on line. Please do not bring equipment into the hospital or GP practices for returning.
Remember all changes should be made slowly and gently. You should always pay heed to your new hip. Everyone recovers at different rates so please do not compare yourself to others. You are all individuals.
It will often take up to 12 months for full recovery from your hip replacement surgery to gradually take place.
Dressing Aids
Following a Total Hip Replacement it is essential to follow the hip precautions, therefore you will be required to purchase an reaching aid and long handled shoe horn prior to your admission. This will help you to dress independently. A sock aid may also be beneficial if you have no one to assist at home. Please bring these with you for your hospital stay. These are widely available from retailers including and specialist mobility shops.
Please be aware these items are no longer provided by the hospital or Social Work Department.
Points to consider when choosing a Reacher:
- Grip and comfort: Choose a Reacher with a comfortable squeeze handle that fits well in your hand. Avoid handles that are too small or don’t spread the pressure evenly across your fingers, as these can be painful to use.
- Length: Reachers come in different lengths, typically from 46cm (18”) to 81cm (32”). Make sure the length suits your height and intended use — if it’s too long or too short, it may be awkward to handle.
- Price: Prices usually range from about £6 to £19. The most expensive option isn’t always the best; focus on comfort, grip, and suitability for your needs.
Points to consider when choosing a Sock Aid:
- Handles: Sock aids with ribbon handles are usually more comfortable than rope handles, which can dig into your hands when pulling.
- Plastic sock aids: If using a plain plastic sock aid, dust it lightly with talc powder. This reduces the risk of your foot sticking to the plastic surface.
- Gutter style sock aids: These are shaped to the contours of your foot, making it easier to slide the sock on compared to flat versions.
- Sensitive feet: If you have fragile skin or reduced sensation in your feet, look for a sock aid with a softer protective layer for added comfort.
Points to Consider for Sock Aids
- Ribbon Handles: Consider a sock aid with ribbon handles rather than rope, as this can be less painful when wrapping around your hands.
- Plastic Sock Aid: If you’re using a plain plastic sock aid, dust it with a little talcum powder to reduce the risk of your foot sticking to the surface.
- Gutter-Style Sock Aid: A gutter-style sock aid, shaped to the contours of your foot, may make it easier to slide on compared to a flat version.
- For Sensitive Feet: If you have altered sensation or fragile skin, choose a sock aid with a softer protective layer for added comfort.
You can also find demonstration videos online by searching for: “Hip precaution dressing techniques” or “Lower body dressing after hip replacement.”
Useful Information & Contacts
What to bring to hospital
- Day clothes and nightwear – we recommend loose fitting clothing and underwear
- Comfortable flat shoes (not flip-flops or mules) – remember your feet may swell after the operation
- Toiletries – towels will be provided
- All current medications in original containers – this allows us to identify them
- Any mobility aids (clearly labelled with your name) – such as sticks, crutches or wheelchairs you normally use
- Entertainment (book, tablet, phone) – your hospital bed will have a TV and WiFi is available
Avoid bringing valuables. Remove jewellery, nail varnish, and make-up before surgery.
Contacts
- Arthroplasty Service (advice line): 01324 567328 or 01324 566621
- Arthroplasty Appointments: 01324 566249
- Arthroplasty Education Group: 01324 566413
- Occupational Therapy: 01324 567435
- Physiotherapy (Ward): 01324 567537
- Pre-Operative Assessment: 01324 566464
- Hospital Switchboard: 01324 566000