This page is designed to help you understand the process of having a knee joint replacement. It outlines what to expect before, during, and after surgery. Please read it carefully and bring it with you to all hospital appointments related to your knee replacement.
If you have any questions, please ask your Orthopaedic Consultant, Registrar, Doctors, Nurses, or Therapists.
In this section:
Knee Joint Replacement Potential Risks and Complications Expected and Potential Outcomes Arthroplasty Service & Appointments Nursing Care Pharmacy Physiotherapy Occupational Therapy Going Home & Transport Dressing Aids Useful Information & Contacts
Knee Joint Replacement
Your knee may need replacing for a number of reasons. The most common reason being arthritis sometimes called ‘wear and tear’. The problems this can cause includes:
- Pain
- Difficulty walking
- Not able to sleep well
- Stiffness
However the main reason for surgery is to help people who are experiencing ongoing severe pain and reduced function. The operation is performed to relieve pain and deformity.
There are several types of implant, and your surgeon will decide whether you need a partial or total replacement based on your individual needs.
The operation usually lasts 45 minutes to 1.5 hours (longer if it is a revision). You will spend some time in recovery before being transferred to the ward.
Most patients go home once they are well enough and have completed physiotherapy and occupational therapy assessments – sometimes on the same day.
Like all major surgery, knee replacement carries risks, including infection, blood clots, pain, swelling, loosening of the implant, and a very small risk of death. Anaesthetic risks are explained in the You and Your Anaesthetic booklet.
Please read all the information provided and ask your team any questions – there are no silly questions.
Potential Risks and Complications
Precautions are taken to try to minimise the risk of infection. The use of antibiotics during and after surgery and the use of a dedicated orthopaedic theatre are examples of those precautions. Despite this there remains a small risk of wound infection. If you, the district nurse or your GP suspect a wound infection please contact our service immediately.
Common signs of infection include:
- Redness around the site of your wound
- Wound discharge or leakage. Wound leakage may occur in the first few days following surgery and may be normal
- Increase in heat and/or swelling
- Increased body temperature (above 38 degrees Celsius)
Late infection can occur many years after your operation. This is often detected by the patient experiencing pain in the knee joint. If late infection is detected this might result in revision surgery to replace/remove the knee joint.
Your Surgeon may request further investigations to confirm infection.
You should note that if you are found to have infection before your knee replacement surgery, your operation will be delayed until you are free of infection. This is to reduce the risk to your ‘new’ knee joint.
As mentioned during your pre-assessment visit, it is very important that you have no breaks in your skin-including deep scratches, any broken teeth or other dental issues, ingrown nails, or other signs of infection such as urinary infection, cold or sickness.
If you develop any of the above following your pre-assessment please let us know prior to your admission for your surgery on 01324 566464.
Thrombosis (blood clot) in the legs or pelvic veins is called deep venous thrombosis (DVT). A thrombosis in the lungs is called pulmonary embolism (PE).
Common signs of DVT:
- Swelling in the thigh, calf or ankle that does not improve with elevation of the leg
- Pain, tenderness and heat in the calf muscle
- Common signs of PE:
- Sudden shortness of breath
- Chest pain or pain between the shoulder blades
- Sweating/confusion
- Feeling faint or unwell
You should call ‘999’ if you suspect a pulmonary embolism as this is a life threatening emergency.
Certain actions are taken to reduce the risk of DVT and PE and are discussed later in the booklet. The risk cannot be completely removed.
This is rare but can give rise to pain in the leg or weakness of some muscles. It can make walking difficult. This is often temporary and will improve over a number of weeks or months. However it can be permanent.
Sometimes patients can lose a large amount of blood during the operation. If this happens you may require a blood transfusion. Like any medical intervention it will only be offered if necessary.
You may find that after your surgery you cannot flex (bend) or extend (straighten) your knee as well as you would like to. IT IS VITAL THAT YOU PERFORM YOUR EXERCISES AS SOON AS POSSIBLE AFTER YOUR OPERATION AND TO CONTINUE THEM WHEN YOU ARE AT HOME.
If you cannot flex your knee beyond 80 degrees your Consultant will be informed. You may be advised to undergo a ‘manipulation under anaesthetic’ of your knee. This will only be offered if it is thought that it might help improve your knee movement. It will involve further anaesthetic and stay in hospital. As with any surgical procedure it carries a degree of risk.
Despite the best of efforts there is a small risk that your knee movement does not improve or move as well as you would like.
Most knee replacements will last between 10-15 years. After around 15 years 25% will appear loose on x-ray and 5-10% will become painful and require revision surgery.
Knee replacement surgery carries a small risk of death. Your Surgeon will be happy to discuss this with you.
Your Surgeon will try to ensure that your legs are of equal length. However if the damage to your bone is too extensive this may not be possible. This is rare but if it happens a small shoe insert or heel raise can be provided.
Incidence of dislocation of the knee joint is very rare. Signs of dislocation are:
- Sudden onset of severe pain
- Unable to weight bear or move the leg.
Expected and Potential Outcomes
During your stay in hospital you will be part of the ‘Enhanced Recovery after Surgery’ (ERAS) programme. The term enhanced recovery is used to describe an approach to performing joint replacement surgery and promoting recovery. The evidence shows that the approach taken delivers better outcomes and a better experience of care for patients requiring surgery.
Swelling of the foot, ankle and knee is very common following knee replacement surgery. This may persist for many months. You have little or no swelling when you first get up in the morning but find that the swelling increases as the day progresses.
Some heat around the knee is usually noted and is caused by increased blood flow through the tissues during healing. Bruising can also be extensive and run the length of your leg.
To ease heat and swelling you can try the use of ice over the knee. Please do not apply ice or very cold substances directly to the skin as this can cause skin burns. The ice pack can be left in place for 10-15 minutes at a time and then should be removed for a couple of hours before using again. Elevating your leg for a period of time can also help to reduce swelling.
You can expect pain around the knee and anywhere along the length of the leg. The pain is due to to the surgical procedure and manipulation of the leg during surgery.
Many patients report that night time is a particular time that they struggle to control pain and discomfort.
You can expect pain to take approximately 3-6 months to gradually improve. You should use analgesia regularly and may need to do so for up to 12 weeks after your surgery.
Around 1 in 4 people can experience ongoing pain despite surgery.
Occasionally, slight numbness around the scar or part of the leg can happen but this is not anything to worry about. Typically you will experience a numb area on the outer side of your operated knee, lateral to your scar. This is usual and will not affect your knee.
It is common for many surgical patients to become constipated in hospital. The reasons for this include surgery, fasting before surgery, change in diet, effects of medication, lack of fluid intake and reduced physical activity. If your bowels do not move as often as normal do tell your nurse. A laxative may be prescribed until your bowel function returns to normal.
You may feel nausea (sickness) or actually vomit after your operation. In this case you can be offered anti-sickness medicines and your painkillers may be reviewed.
You may suffer from indigestion which may be as a result of medication. While it is probably nothing to worry about you should go and see your GP. Your painkillers may need to be changed, or rarely, it can indicate a problem with your heart.
Arthroplasty Service & Appointments
The Arthroplasty Service is nurse-led and provides support before and after your surgery.
- Available Monday to Friday, 8am–5pm
- You can call and leave a message; calls will be returned as soon as possible
- You will attend an Arthroplasty Education Group before your surgery, which lasts about an hour and prepares you for what to expect
- A follow-up clinic appointment is arranged for 6 weeks after your operation to check your wound, movement, and walking progress
Nursing Care and Hospital Recovery
Nursing staff will guide and support you throughout your hospital stay.
- Visiting hours: 11.30am–8.00pm daily (maximum 2 visitors at a time; please avoid bringing babies).
- On surgery day, you may not reach the ward until late. Next of kin should phone after 4pm to check before visiting.
- To help staff, please avoid calling before 11am and nominate one family member as the main contact.
Following surgery you will be transferred to the Theatre Recovery Area where specially trained nurses will remain with you while you recover from the anaesthetic.
Once awake and alert your Ward Nurse will escort you back to the ward.
You will most likely find the following:
- A cuff around your arm, which will record your pulse and blood pressure at regular intervals
- Oxygen mask
- A drip (intravenous infusion) will be attached to your arm. You will have clear fluids or possibly a blood transfusion in progress.
Nurses will assist you with personal hygiene where necessary. The ward will provide towels: however, you are expected to supply your own washing cloth/sponge, toiletries, nightwear and daytime clothing. Please do not bring flip-flops or mules. Closed foot wear should be worn to prevent trips or falls. Please advise staff when you need to use the toilet, you will be assisted as necessary. You can alert staff by using the nurse call buzzer. Buzzers are situated by the beds.
With the assistance of staff you may attempt to get out of bed the same day as surgery. You should NOT attempt to get out of bed on the first occasion on your own. Many people feel faint and light headed on the first attempt. This is because your blood pressure drops and makes you feel unwell.
Your new joint should not cause discomfort but you may experience some pain from the actual surgery itself.
- Advise nursing staff whenever you experience pain. It is vital that your pain levels are under control so that you can move and do your exercises
- You do not have to wait until drug rounds should you require painkillers
- Relevant pain relief would be administered
- As pain reduces tablets are usually adequate
- Some painkillers can be dissolved in water if you have problems swallowing tablets.
- The outer bandage will be removed on day 1 after your operation. The primary dressing (next to the wound) will be left in place for up to 2 weeks undisturbed if possible to reduce the risk of infection
- The nurse will only clean your wound and change the dressing if required, for example, if there is excessive wound soakage on the dressing
- The district nurse will attend to remove clips and check the wound at 12-14 days
- A further dressing will be applied for a further week and this can be removed by the patient at the 3 week mark.
You may have a special wound dressing that has a battery unit attached. When the batteries run out around 5-7 days, the dressing will remain in place as a normal dressing would, until the district nursing team remove at 2 week check.
You may develop bruising and swelling on the operated leg. This is very common and may persist for several months after surgery. The swelling may be better in the morning and increase as the day progresses. Swelling may be evident along the length of the operated leg as can bruising. You will experience a degree of warmth/heat around the knee and this is part of the healing process.
Your wound will be vertical over the front of your knee and approximately 6 inches in length. It should eventually fade to a thin white line.
Very occasionally problems may arise as a result of surgery:
To avoid constipation once you have recovered from the anaesthetic:
- Drink plenty of fluids
- Eat fruit and vegetables
- If you feel constipated and/or your bowels have not moved for 2 days advise your nursing staff or GP if you are at home
- Oral medications (laxatives) or rectal preparations (enema or suppositories) will be available for you on prescription if required.
Measures are taken to prevent blood clots e.g.
- Ensure you are mobilising regularly, as able, with the support of your walking aids
- Anticoagulant (blood-thinning) medicine will be given whilst in hospital and on discharge if required
- Ankle and leg exercises as described by the physiotherapist will be encouraged.
Very occasionally this complication may still arise.
When you are still on the ward, please advise your nurse or doctor if any of the following occur:
- Pain at your calf (lower leg)
- Swelling and/or increased tension at your calf
- Pain in your chest
- Shortness of breath.
If these signs occur when you are at home please contact your GP immediately.
Thrombus (blood clot formation) is treatable with medication.
Pharmacy and Medicines
Please bring an adequate supply of your medicines into hospital when you attend the pre-admission clinic and when you attend for surgery. This will ensure the healthcare team can determine what medicines you normally take and your medicines are available on the ward.
Your regular medicines will continue where appropriate and you are likely to be given some medicines to relieve pain, prevent infection, prevent blood clots, or to treat nausea or constipation.
Knee surgery increases the risk of blood clots. To reduce this, you may be prescribed a short course of blood-thinning tablets (such as rivaroxaban) or injections. These must be taken exactly as prescribed.
Seek medical help if you notice:
- Calf pain or swelling
- Chest pain or sudden breathlessness
- Unusual bleeding (e.g. blood in urine/stool, nosebleeds lasting >5 mins, coughing blood, heavy cuts that won’t stop bleeding)
Rivaroxaban tips:
- Take with food
- Don’t double up if you miss a dose
- Inform your GP if you feel dizzy, faint, or notice side effects
- Tell your doctor about any other medicines, as some increase bleeding risk
You may be prescribed a short course of antibiotic injections around the time of surgery to prevent infection. Occasionally you may require a longer courseof antibiotics if you develop an infection following surgery. Again it is important to complete the course even if you feel well as this will help prevent joint infections. Side effects of antibiotics may include rash or diarrhoea. You should inform healthcare staff if your side effects are troublesome. Please also advise staff if you are allergic to penicillin, for example.
An important part of your care is to ensure that you do not experience excessive pain. A range of painkilling medications are used. Most patients will receive paracetamol, which is a very effective and safe painkiller on its own or in combination with other painkillers. You are advised to take these on a regular basis until the pain is negligible.
You are also likely to be prescribed a stronger opiate painkiller according to your requirements. Opiate painkillers include codeine, dihydrocodeine, tramadol, morphine and oxycodone. These may be given regularly or when you need them in either tablet or liquid form. Other painkillers are sometimes added if you have inflammation or nerve pain.
It is particularly important to take adequate pain relief before movement and physiotherapy. Your painkillers will be rationalised as your pain improves. If you are in pain, please do not suffer in silence and ask your nurse for assistance.
Side effects you may experience with the stronger (opiate) painkillers include drowsiness, nausea and constipation. These side effects can be managed with other medicines or by taking the painkillers at a lower dose or only when needed.
It is common for many surgical patients to become constipated in hospital. The reasons for this include: the effects of surgery, fasting before surgery, change of diet, effects of painkillers and through lack of fluids and reduced physical activity. There is therefore no reason to worry if your bowels do not move as often as normal, but do advise staff if you feel uncomfortable and would like laxatives to help. These can usually be stopped within days when your bowel function returns to normal.
You may feel nausea (sickness) or actually vomit after your operation. In this case you can be offered anti-sickness medicines and your painkillers may be reviewed.
Your pharmacist, doctor or nurse can offer advice and help you with a range of potential medication problems and to respond to any other symptoms that may trouble you.
When You Go Home
Your doctor or nurse will arrange any medicines you need to take home. This process can take a few hours. You’ll usually receive a week’s supply of painkillers and your full course of blood-thinning tablets. Contact your GP if you need more.
Most people have no issues with side effects, but it’s important to take all medicines as prescribed to aid recovery and prevent complications.
Physiotherapy: exercises, walking & stairs
You will receive physiotherapy as part of your rehabilitation while you are in hospital, and occasionally as an out-patient once you are discharged home
if appropriate. Physiotherapy will start the same day as surgery.
Before your operation
You can practice your physiotherapy exercises before your operation providing it is comfortable to do so. You should stop any exercise that increases your pain. If you find the exercises difficult then try increasing the repetitions more gradually.
Post Operation
The rehabilitation process begins immediately after your operation. This is just as important as the operation itself, and will involve a lot of hard work. All members of the ward team will be involved to help you gain your full potential. We will assist you with the exercises outlined in this booklet and ensure that you are able to walk safely and well.
Your knee will be swollen for up to 6-12 weeks after surgery. It is not unusual to feel heat at your knee during this time.
Because you have had an anaesthetic and are not as active as normal, it is important that you perform some deep breathing exercises to help keep your lungs clear.
- Take a deep breath in through your nose until you feel that your lungs are full of air, hold for a second then sigh the air out through your mouth. Keep your shoulders relaxed.
Perform this exercise 3 times every hour while you are awake.
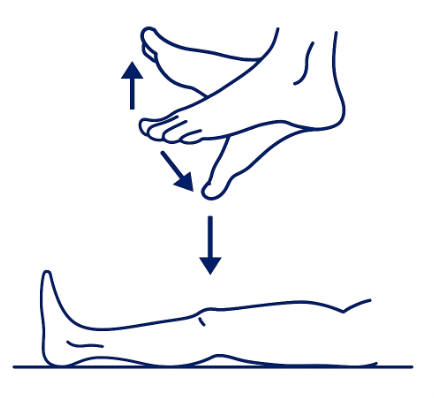
These exercises will improve your circulation while you are immobilised in bed. This will reduce the risk of developing a blood clot.
Point your toes down towards the end of the bed and then pull them up towards you as far as you can. You should feel your skin and calf muscles tightening as you do these exercises.
Pull your foot up towards you, then push the back of your knee down onto the bed. You should feel your kneecap tightening. Hold for 5 seconds, then relax.
Tighten your buttocks together as firmly as you can. Hold for 5 seconds, then relax.
Perform 20 of each exercise every hour while you are awake.
Movement Exercises
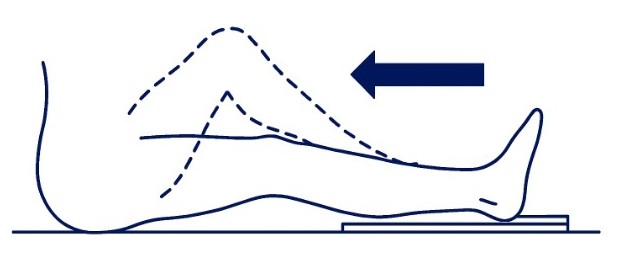
The following exercises are designed to improve how far you are able to bend (Flex) your knee. We normally aim to achieve 80 degrees while you are in hospital. It is also vital that you are able to fully straighten (extend) your knee.
The exercises are performed initially on a sliding board to minimise resistance. Place the sliding board under your leg and the tubigrip “doughnut” under your heel. Slowly bend and straighten your knee as far as possible. Aim to get a little further each time. The sliding board is NOT provided on discharge from hospital.
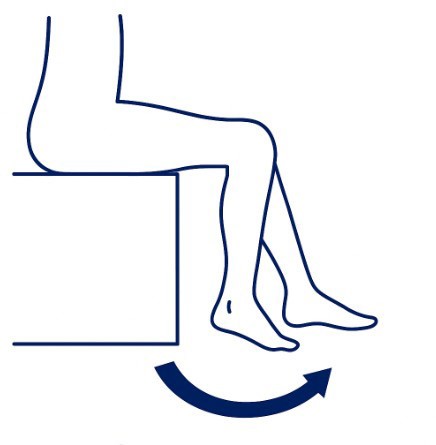
Sit comfortably in your chair or at the side of your bed. With your foot on the floor, try to slide your foot back as far as possible. You can use your UNoperated leg to assist. Make sure that you keep your bottom flat down as you bend to avoid cheating. (It is natural to feel some “pulling” at your wound with these exercises).
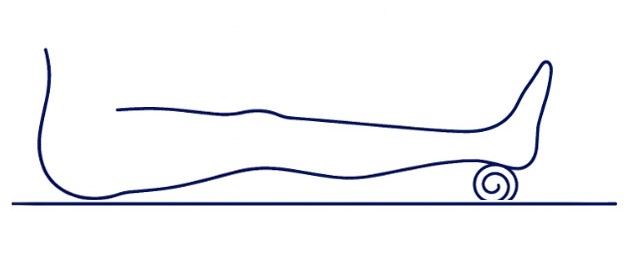
Place a folded towel under your heel with your leg straight. Gravity and the weight of your leg will help to stretch out the back of your knee.
Never rest with a pillow under your knee. This can encourage tightness to develop at the back of the joint and make it very difficult for you to fully straighten your leg.
Strengthening Exercises
Perform these exercises while sitting on top of your bed.
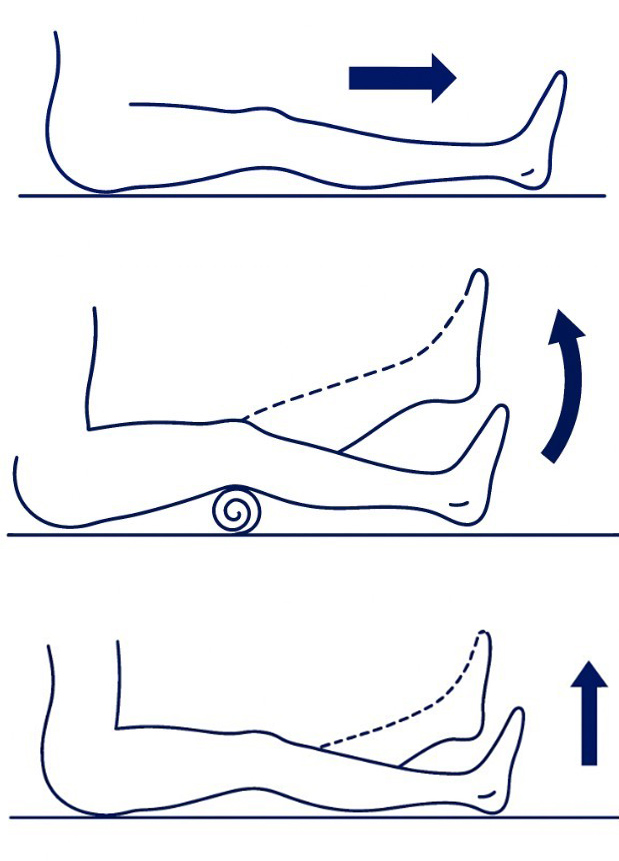 Pull your foot up towards you, then push the back of your knee down onto the bed while aiming to tighten your kneecap. Hold for 5 seconds then relax.
Pull your foot up towards you, then push the back of your knee down onto the bed while aiming to tighten your kneecap. Hold for 5 seconds then relax.- Place a rolled up towel under you knee. Pull your foot up towards you, press the back of your knee onto the towel then try to lift your heel off the bed. Aim to get your knee completely straight. Hold for 5 seconds then slowly lower your heel back down onto the bed. Do not lift your knee off of the towel.
- Pull your foot up towards you and tighten your knee as in the first exercise, then try to lift your leg about 15cm (6 inches) while keeping your knee as straight as you can. Hold for 5 seconds then slowly lower your leg back onto the bed.
Walking
You will normally get out of bed and start walking as soon as possible after surgery. Initially you will be given a walking frame to start the process of getting back onto your feet. This will then change to walking sticks /crutches as your mobility improves. Once you feel confident with your walking aid you should aim to take several short walks throughout the day.
Use the following pattern when walking with your frame/sticks:
- Move frame/sticks forward
- Step forward with operated leg followed by UNoperated leg
When you are ready you will normally progress from the walking frame onto 2 sticks.
Once you are at home and gaining in confidence and strength you can consider weaning off your sticks. You should only do this if you are no longer limping. You should begin by reducing down to the use of one stick. That stick should be held in the opposite hand to the operated leg. The sequence of walking with one stick should be to move the stick and operated leg forward and then walk through with your unoperated leg. Please note that everyone will progress at different rates.
Once you are confident with your sticks, your physiotherapist will show you how to safely go up and down stairs. The method is as follows:
Down
Place the sticks down onto the stair below, step down with the operated leg, followed by the UNoperated leg
Up
Step up with the UNoperated leg first, then step up with the operated leg followed by the sticks
This is the easiest and safest method for negotiating stairs and places the least amount of strain on your new knee.
Please note that there is reduced Physiotherapy and Occupational Therapy services at the weekend. Patients must take responsibility to carry out exercises without the need for instruction from nursing staff. You must therefore do your exercises at the weekends as shown previously by physiotherapy staff. Nursing staff will be available for advice.
You can expect a stay in hospital of 1 day.
Your knee will continue to get stronger and more flexible, provided you continue with your exercises at home. The hard work should not stop just because you are no longer in hospital.
It is vital that you perform your exercises 3-4 times a day at home and attempt a walk every day. You should gradually build up the distance you walk within your tolerance.
Occupational therapy & Knee Precautions
The aim of Occupational Therapy is to enable people, including those who have had surgery to be as independent as possible with their everyday lives.
Occupational Therapy is part of your rehabilitation. Initially the Occupational Therapist will discuss with you any day to day difficulties you may have had and how to remain independent following your surgery.
Whilst you are in hospital the Occupational Therapist will assess your ability to manage everyday activities safely and independently, so that you will be able to manage these yourself at home. These may include:
Dressing
Within a couple of days you should be able to put on your lower garments unassisted. If you are experiencing difficulties the Occupational Therapist will be able to discuss these difficulties and offer practical advice.
Personal Activities of Daily Living
Before you are discharged from hospital, an Occupational Therapist will check your ability to perform everyday activities such as getting in and out of bed, getting on and off the toilet and coping with bathing. You will find it easier to strip wash or shower immediately following surgery. It is advised NOT to have an immersion bath too soon because you may be too weak to raise yourself from the bottom of the bath.
Domestic Tasks
Before you come into hospital you may want to consider organising friends or relatives to help you in the short term with shopping and other domestic tasks. You should not attempt any activities which involve kneeling until you feel comfortable.
You can expect to be able to return to carrying out activities in the kitchen as you did prior to your operation and an Occupational Therapist will assess your capabilities before discharge. Advice will be given on how to cope with various kitchen tasks whilst you are still dependent on walking aids.
Leisure Activities
Your Orthopaedic consultant surgeon will advise you about recommencing activities such as swimming, bowling, dancing, gardening etc. Do ask him or her for guidance. Initially all these activities should be undertaken gently and without excessive effort.
Going Home & Transport
After knee replacement surgery, most patients stay around 1 day (sometimes less if recovery is quick). Discharge planning begins at your pre-assessment and continues during your stay to make sure you go home safely. If you need extra rehabilitation, you may be transferred to another ward or community hospital before discharge.
domestic tasks. You should not attempt any activities which involve kneeling until you feel comfortable.
You can expect to be able to return to carrying out activities in the kitchen as you did prior to your operation and an Occupational Therapist will assess your capabilities before discharge. Advice will be given on how to cope with various kitchen tasks whilst you are still dependent on walking aids.
Home Care
You’ll need some help in the first few weeks:
- Arrange for family/friends to help with shopping and housework.
- If this isn’t possible, let staff know at your pre-op assessment or on admission so support can be arranged.
Transport
- You must not drive until your knee can safely control the vehicle and you are pain-free.
- Do not drive until after your 6-week clinic review, and only with your Consultant’s or Arthroplasty Service’s approval.
- You don’t need to inform the DVLA, but you must inform your insurance company.
- Arrange for family or friends to take you home after surgery.
Returning to Work
- Discuss your return with your employer and GP before surgery.
- A phased return or lighter duties may be recommended.
- Allow for around 12 weeks off work.
- Ask your pre-assessment nurse if you need a fit note (sick line).
Dressing Aids
Following a Total Knee Replacement there are no precautions to follow however you many find some of these items beneficial, therefore you may wish to purchase prior to admission.
Please be aware these items are no longer provided by the hospital or Social Work Department.
Reaching Aid
Points to consider when choosing a Reacher:
- Grip and comfort: Choose a Reacher with a comfortable squeeze handle that fits well in your hand. Avoid handles that are too small or don’t spread the pressure evenly across your fingers, as these can be painful to use.
- Length: Reachers come in different lengths, typically from 46cm (18”) to 81cm (32”). Make sure the length suits your height and intended use — if it’s too long or too short, it may be awkward to handle.
- Price: Prices usually range from about £6 to £19. The most expensive option isn’t always the best; focus on comfort, grip, and suitability for your needs.
Sock Aid
Points to Consider for Sock Aids
- Ribbon Handles: Consider a sock aid with ribbon handles rather than rope, as this can be less painful when wrapping around your hands.
- Plastic Sock Aid: If you’re using a plain plastic sock aid, dust it with a little talcum powder to reduce the risk of your foot sticking to the surface.
- Gutter-Style Sock Aid: A gutter-style sock aid, shaped to the contours of your foot, may make it easier to slide on compared to a flat version.
- For Sensitive Feet: If you have altered sensation or fragile skin, choose a sock aid with a softer protective layer for added comfort.
You can also find demonstration videos online by searching for: “Hip precaution dressing techniques” or “Lower body dressing after hip replacement.”
Useful Information & Contacts
What to bring to hospital
- Day clothes and nightwear – we recommend loose fitting clothing and underwear
- Comfortable flat shoes (not flip-flops or mules) – remember your feet may swell after the operation
- Toiletries – towels will be provided
- All current medications in original containers – this allows us to identify them
- Any mobility aids (clearly labelled with your name) – such as sticks, crutches or wheelchairs you normally use
- Entertainment (book, tablet, phone) – your hospital bed will have a TV and WiFi is available
Avoid bringing valuables. Remove jewellery, nail varnish, and make-up before surgery.
Contacts
- Arthroplasty Service (advice line): 01324 567328 or 01324 566621
- Arthroplasty Appointments: 01324 566249
- Arthroplasty Education Group: 01324 566413
- Occupational Therapy: 01324 567435
- Physiotherapy (Ward): 01324 567537
- Pre-Operative Assessment: 01324 566464
- Hospital Switchboard: 01324 566000
More information about surgical procedures and what to expect can be found on NHS Inform.