Transformation – Research & Development, service design & innovation
Innovation within NHS Forth Valley supports the development, funding and implementation of impactful innovation projects which have the potential to transform health and social care and address demographic, economic and workforce challenges.
NHS Forth Valley is involved in a number of regional and national forums, including the West of Scotland Regional Innovation Hub, a member of the Test Bed innovation model, and leads the national Dermatology AI Consortium.
Locally the Innovation team work with our growing number of local innovators to scan and attract opportunities for innovation and colleagues are encouraged to submit proposals. Please refer to the section on “How to undertake a project improvement project” for more details.
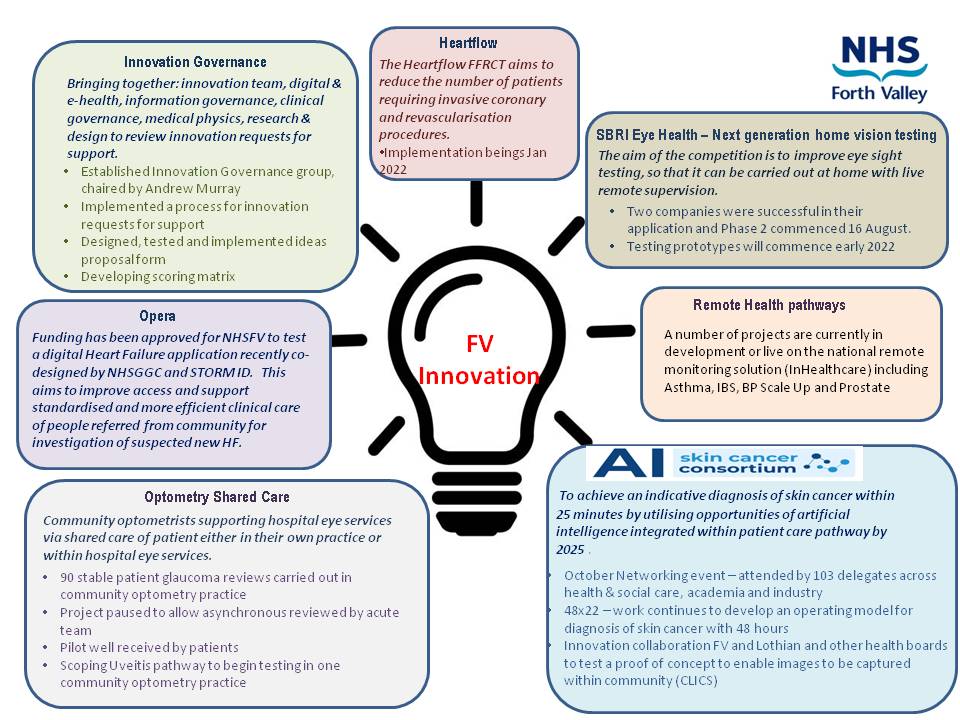
The diagram below highlights the current projects approved for implementation within NHS Forth Valley.
- Ophthalmology (Optometry Shared Care) – Establish a shared care programme for patients with stable Glaucoma, macula and uveitis conditions.
- Open Eyes – Open Eyes is a electronic patient record for Ophthalmology.
- OPERA – A digital Heart Failure application to support standardised and more efficient clinical care of people referred from the community in NHS Forth Valley (NHSFV) for investigation of suspected new Heart Failure.
- Heartflow – Trialling the use of HeartFlow technology for patients with evidence of coronary disease on CT imaging.
- RHM: Asthma – The asthma remote health pathway has been, developed to allow remote monitoring of severe / difficult to control asthma patients by their specialist respiratory nurse / consultant.
- RHM: IBS – The IBS remote health pathway has been, developed to support patients requiring specialist dietary therapy to help manage their symptoms.
- Florence: project support – Increasing the number of people using technology, enabled care, to achieve better control and self-management of blood pressure and fewer associated GP/Practice Nurse appointments. Secondary objectives are to reduce antihypertensive prescribing and prevent cardiovascular problems, stroke and renal problems.
- Dermatology AI 48×22 – The project will provide the diagnosis of skin cancer within 48 hours by the end of 2022.
- Dermatology AI 25×25 – By 2025, an indicative diagnosis of skin cancer in Scotland is, achieved within 25 minutes by utilising opportunities of artificial intelligence (AI) integrated within patient care pathway.
- Realistic Medicine – an approach to healthcare that aims to put the patient at the centre of decisions made about their care. Shared decision- making and a personalised approach to care are key elements of practising Realistic Medicine. Our aim is to provide you with access to learning and practice support tools to help you embed Realistic Medicine into your daily practice.
Quality Infrastructure & Improvement
- Mental Health Improvement Programmes – Taking a QI approach to deliver successful and sustainable improvements to mental health care pathways. Reducing waiting times by improving pathways to balance the workload associated with referrals to the demand for care (Phase one: Anxiety, Drugs and Alcohol, Early Intervention in Psychosis and Dementia).Mental health improvement programmes will also include value management and the implementation of the MAT standards.
- Access QI – Improving access to planned care pathways – The Access QI programme, is a collaboration between Healthcare Improvement Scotland (HIS) and NES, and participating health boards which brings together a core team, data analyst and quality improvement (QI) coach – to focus on improving a care pathway.The team works together to:
- work on an identified pathway
- identify improvement opportunities
- plan and undertake improvement work to deliver sustainable, positive changes in patient outcomes
- Teams based approach to quality – A value management approach bringing cost and quality data to the point of care to drive sustained improvement. Teams are supported with 1:1 coaching and team education to develop their QI capacity and capability to improve safety, quality and experience for staff and patients.
- Primary/secondary care interfaced group – commissioned projects – to be determined
- Community AHP pathways – core project team identified, identify aim and agree approach. Deliver training in quality improvement and project management.
- Safety Improvement Workstream Development – Launched in 2008, the Scottish Patient Safety Programme, is a national quality improvement programme that aims to improve the safety and reliability of care and reduce harm. Working collaboratively with the Acute Care Team at Healthcare Improvement Scotland, our aim is to reduce harm across three priority areas in Forth Valley:- Deteriorating patient, Falls and falls with harm, Venous thromboembolism prophylaxis.Engaging as a member of the National Acute Care Collaborative, selected wards will apply a teams-based approach to quality to develop a deep understanding of their current system and challenges. They will take forward new ideas, applying QI principles to improve the reliability of existing and new safety processes. Learning will be shared at both local and national level, celebrating successes as they progress.
- Primary Care – Primary Care Improvement Plan – reduce GP workload: improve for patients to access right primary care first time.
- Creating the conditions for a culture of joy in work – embed the principles of IHI Joy in work, improve staff experiences, monitor sickness, absence and turnover.
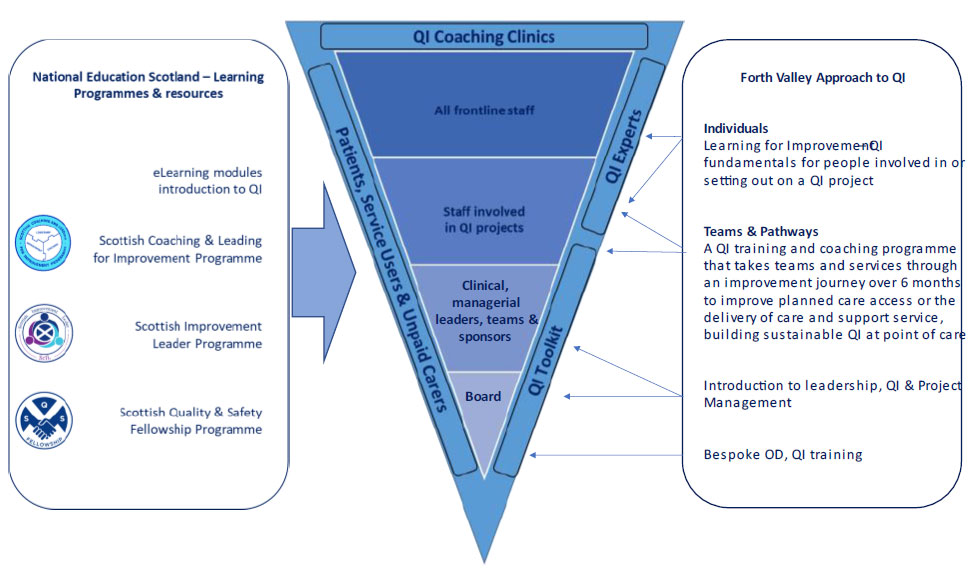
- Building Capacity and Capability – Continuous quality improvement and significant transformational change are two levels of change that we will continue to use and support. Guided by evidence, our continuous quality improvement approach includes what staff have learned from what has and has not worked and from taking part in learning opportunities, programmes and projects. Continuing to develop staff confidence and skills in improving quality through externally funded programmes and projects, we will also explore quality internships and other ways of utilising the skills and talents of people who already have a level of experience in quality improvement. Where helpful and possible we will also seek and, or commission support from external partners.
- Care Pathway Development Programme – Using Quality Improvement to deliver successful and sustainable improvements to care pathways. Reducing waiting times by improving pathways to balance the workload associated with referrals to the demand for care.
- Scottish Access Collaboration/modernising patient pathways programme – service delivery groups: each service group completed baseline gap analysis, benefit realisation plans in place and learning systems developed and delivered.