Pregnancy With Diabetes
Managing pregnancy with diabetes requires careful planning and close monitoring, but with the right guidance and support, a healthy pregnancy is entirely possible. This page is dedicated to providing you with essential information, tips, and resources to navigate this journey with confidence.
If you are planning to become pregnant in the next 6 months then contact the Forth Valley Diabetes Nurses so we can discuss this with you and support you.
We will:
- Discuss what to expect during your pregnancy.
- Discuss the best contraception to use until blood glucose and Hba1c are at pregnancy targets.
- Recommend blood glucose levels of less than 5.5mmols before meals, and less than 8mmols 2 hours after meals. Recommend your Hba1c be less than 48mmols prior to conception and during pregnancy to reduce the risks to both mum and baby. We can discuss various options to help you achieve these targets.
- Ensure you are not on any medication that may cause problems in pregnancy.
- Ensure you have access to our Specialist Diabetes Dietitians.
- Advise you take folic acid 5mgs (prescription only) for at least 3 months prior to conception and until 12 weeks pregnant.
- Advise you take Vitamin D 10mcg throughout your pregnancy.
- Ensure that all your diabetes screening is up to date, and discuss what to expect if you have any complications from your diabetes.
- Take blood to check your thyroid function is normal before becoming pregnant.
- Ensure you have help to stop smoking or drinking excessive alcohol before becoming pregnant.
- Ensure you have registered with MyDiabetesMyWay so you can access all your diabetes records.
- Ensure you are able to download your meter
- Discuss the risks of inheriting diabetes.
- Discuss technologies available which may help keep BG in target.
- Contact the Forth Valley Diabetes Nurses to arrange a review.
- Ensure you have a blood glucose meter, so you can test before and 2 hours after meals and before bed.
- Aim for blood glucose levels of less than 5.5mmols before meals and less that 8mmols 2 hours after meals and for your Hba1c to be less than 48mmols.
- Arrange an appointment with your Community Midwife (via your GP practice). They will also book your first scan at around 12 weeks.
• Stop smoking & drinking alcohol. - Take folic acid 5mgs (prescription only) until 12 weeks pregnant.
- Take Vitamin D 10mcg throughout pregnancy (you can take this as a pregnancy multi-vitamin).
- Ensure you have blood ketone test strips (check the expiry date).
- Ensure you have a glucagen kit (check the expiry date).
- Ensure you have registered with MyDiabetesMyWay so you can access all your diabetes records
- Ensure you are able to download your meter
- Your Diabetes Specialist Nurse will ensure you are seen in the correct antenatal clinic
Gestational Diabetes
This is a type of diabetes that affects pregnant women, usually during the second or third trimester. In most cases gestational diabetes disappears after the baby is born. Gestational diabetes is more common in women who have a higher body weight but it may also develop in other situations. These include the following:
- Having had gestational diabetes in a previous pregnancy
- A large baby in a previous pregnancy (over 4.5 kg/10 lb) or 95th centile and over.
- Being over 40 years old
- A family history of diabetes
- Being of South Asian, Middle Eastern, African or African-Caribbean ethnicity
- diagnosis of Polycystic Ovary Disease (PCOS)
I’m planning a pregnancy and am at risk gestational diabetes, what should I consider?
If you are planning to become pregnant, you can contact the diabetes prevention team at fv.diabetespreventionteam@nhs.scot
We can:
- Discuss what to expect during your pregnancy and importantly what you can do to minimise risk and get you in the best possible place to embark on a pregnancy.
- Make sure you have access to self management programmes for managing your weight and/or physical activity if you’d like to
- Offer help to stop smoking or drinking excessive alcohol before becoming pregnant
- Discuss the risks of GDM for yourself and for your baby
We also:
- Advise you take folic acid 5mgs for at least 3 months prior to conception and until 12 weeks pregnant.
- Advise you take Vitamin D 10mcg throughout your pregnancy.
Contact Us
Antenatal Clinic
Phone: 01324 567094
Dietitians
Phone: 01786 434437
Email: fv.diabetespreventionteam@nhs.scot
You can:
Contact the Booking Bureau on 01324 567 146 or email fv.pregnantfv@nhs.scotYou will find more information on the NHS Forth Valley – Positive Pregnancy Test page.
A community midwife will get in touch with you.
We will:
- Ask a few questions and arrange your first midwife appointment. This will be with your Community Midwife
Then your Community Midwife will:
- arrange for your first scan at around 12 weeks and a review in the Antenatal Clinic at Forth Valley Royal Hospital. They will then invite you to attend a Gestational Diabetes Group Education session where you will receive your blood glucose meter.
- check an HbA1c blood test to check that you have not developed Type 2 Diabetes since your last pregnancy.
- discuss taking Vitamin D 10mcg throughout pregnancy (you can take this as a pregnancy multi-vitamin).We may advise a higher dose at your booking appointment, and will arrange a prescription if needed
Let us know if you would like help to stop or reduce smoking or help to stop drinking alcohol.
During your pregnancy
We will guide you in monitoring your blood glucose levels, helping you to achieve good control of your blood glucose levels throughout your pregnancy. This ensures the best possible outcome for you and your baby.
Over half of women will be able to control their Diabetes simply by alterations to their diet. However some women may need medication.
Growth scans will be arranged from 28weeks gestation with review afterwards by your own Consultant in the antenatal clinic.
If you progress to medication, you will be asked to attend our Diabetes Antenatal Clinic at FVRH. This clinic has a team of professionals to support you which includes an Obstetrician, a Midwife, a Diabetes Specialist Nurse and a Dietitian. This allows you to see whichever health professionals you need to see within our team at one appointment.
When you are diagnosed with GDM you will be invited to attend a group education session. This session lasts around an hour and a half and we’ll talk about:
- what is GDM?
- why it’s important to monitor blood glucose levels and blood glucose targets
- everything you need to know about using your blood glucose meter and getting prescriptions
- how to contact antenatal clinic if you have 3 raised blood glucose readings within 7 days
- the importance of carbohydrate when controlling your blood glucose
- what happens if you need a bit more help after making dietary changes
- when to feed your baby after they are born and colostrum harvesting
- what to expect after your pregnancy
When you have GDM, your body can’t control glucose levels in your blood because you are either not making enough insulin, or the insulin being made is not working properly.
When we eat foods containing carbohydrates, the carbohydrate is digested into glucose in your stomach and it will then travel into your blood stream.
What should happen?
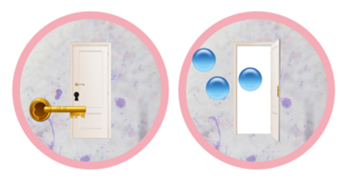
These are cells. Imagine every cell has a lock on it. You need insulin (the key) to unlock the cell door and let the glucose into the cell. Insulin is made in the pancreas.
What happens in Gestational Diabetes?
In Gestational Diabetes, the placenta makes extra hormones which can stop your insulin keys from working properly. Sometimes the insulin key doesn’t work properly in the cell lock. Most often, one insulin key is not enough to unlock the cell door, so we need to make more keys.
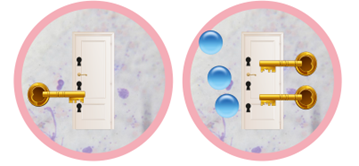
When you have GDM, we recommend that you aim for your plate to look like this:
We recommend that you eat a healthy diet with 3 regular meals, and small snacks if you feel you need them. You can watch how much carbohydrate you are eating and drinking. Aiming for around 150-200g per day (30g to 50g per meal) can be a good guide, but we will discuss this at your GDM group education session and your follow up telephone appointment.
| Starches | Added Sugars | Natural Sugars |
| Bread | Fizzy drinks | Fruit |
| Rice | Cakes | Fruit Juice |
| Pasta | Biscuits | Dried Fruit |
| Potatoes | Chocolate | Milk |
| Pulses | Sweets | Yoghurt |
| Cereals | Cereals | Smoothies |
Foods we haven’t mentioned which would not affect your glucose levels are:
- Fats – spreads, oils, cream, butter
- Proteins – red/white meat, fish, eggs
- Miscellaneous – salads and cheese
Added sugar is only one source of carbohydrate, it is equally important to consider starchy carbohydrates and natural sugars. It is the total amount of carbohydrate which will affect how much your glucose levels will rise. When looking at food labels, it is the total amount of carbohydrate, on the back of the pack which you need to look at, rather than the sugars. Choose wholegrain or high fibre carbohydrates where possible.
To watch a video for information about all the food groups and how to eat a balanced diet, visit Gestational Diabetes and Diet – YouTube
For information in different languages, including easy read and Braille, visit Diabetes information in different languages | Diabetes UK
The Glycaemic index is a scale which shows how quickly a carbohydrate containing food releases its glucose into the blood stream.
Glycaemic Load is a way of showing how quickly foods which are eaten together will release their glucose into the blood stream. Foods are usually eaten together e.g. pasta with a sauce.
Food Pairing is another way to describe glycaemic load. It considers how putting higher fat or higher protein foods with higher carbohydrate foods to slow the release of glucose into the blood stream. It may be better to choose higher protein foods to pair with higher carbohydrate foods, instead of using high fat foods which may cause weight gain. This topic will be covered at the GDM group session and can be discussed further with your dietitian.
You will be given your blood glucose monitor at your GDM group session. We will show you how to use your meter. We will also give you blood glucose targets.
As a reminder, you can watch these videos about how to test your glucose level.
- How to obtain a blood sample using the Agamatrix lancing device
- How to perform a blood glucose test using the WaveSense
You can watch this video about how to upload your readings to the midwives at the ante natal clinic.
Whether you are newly diagnosed or you have had GDM in a previous pregnancy, we will ask you to test your blood glucose 4 times every day.
This allows you to see how well you are controlling your blood glucose levels. It lets you know when you may need to make more dietary changes, and when you will need to ask for help to better control your blood glucose levels.
These are the numbers we need to remember, and what they mean.
Test 4 times every Day:
- Before Breakfast (fasting) with an aim of less than 5.5mmol/l
- 1 hour after Breakfast (post-prandial) with an aim of less than 8.0mmol/l
- 1 hour after Lunch (post prandial) with an aim of less than 8.0mmol/l
- 1 hour after Evening Meal (post-prandial) with an aim of less than 8.0mmol/l
Colostrum is the first milk produced for your baby.
It has lots of nutrients and can help build your baby’s immune system. It is also made just for your baby as it has come from you.
You should only hand express your breast to collect colostrum after 36 weeks of pregnancy. This is called Colostrum harvesting.
You should avoid harvesting if:
- you have ever had a cervical suture
- you have ever had a preterm labour
- you have a low lying placenta called placenta praevia
- you are pregnant with twins, triplets, or more
- you have polyhydramnios (too much fluid around the baby)
There are lots of great reasons to harvest colostrum, but when you have GDM, it is even more helpful to have stored colostrum to offer your baby if their blood glucose goes too low in the first few days after birth.
We will discuss colostrum harvesting further at the group.
To find out more, and to get your Colostrum Harvesting pack, talk to anyone at your ante natal clinic appointment, or phone us on 01324 567094.
During Labour
We will check your blood glucose when you are admitted to labour ward. If your blood glucose is high, we’ll talk you through what happens next.
If you are induced, we may need to support you a little differently, depending on your original birth plan, but we will make sure that we talk you through what is happening and why.
 We recommend that you feed your baby as soon as you can after you give birth. If you feel able and would like to, breastfeeding is the preferred feeding method. If you have collected colostrum, you may also want to offer this to your baby until feeding is established.
We recommend that you feed your baby as soon as you can after you give birth. If you feel able and would like to, breastfeeding is the preferred feeding method. If you have collected colostrum, you may also want to offer this to your baby until feeding is established.
Do I still need to test my blood glucose levels?
You do not need to test your blood glucose levels after you have had your baby unless otherwise advised.
After you have had your baby you will no longer have Gestational Diabetes as this is only present when you are pregnant.
Feeding
If you are planning to breastfeed, do allow as much time as possible for skin to skin contact as this helps release the happy hormone oxytocin which helps with milk production.
After a C section, there can be a delay in milk production. You can ask your midwife for donor breast milk if you would like this for your baby.
If you are planning to formula feed, feed your baby as soon as you feel able, after the baby is born.
Paced feeding is a way of giving your baby more control over their feeds. Babies usually take a small amount of milk, stop for a rest and then take more.
You can help them “pace” their feeds so it mimics the way they would feed if they were being breastfed.
Postnatal Care
You will need to stay in hospital at least 24 hours after you have had your baby. There are many things which will determine length of hospital stay. This will be decided by the team of midwives and doctors supporting you and your baby after you have given birth.
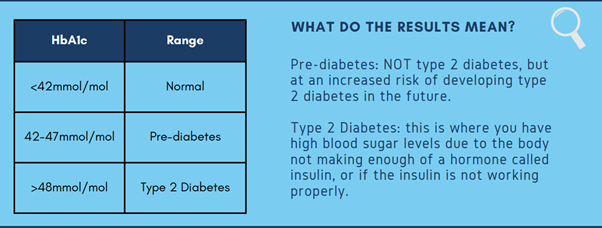
What is an HbA1c test, and when should I be tested?
The HbA1c test is a blood test which measures your average blood glucose levels over the past 8-12 weeks. It tests for Pre-Diabetes and Type 2 Diabetes. You should be invited by your GP to have this test 13 weeks after you have had your baby, and once a year after that.
If you haven’t been invited, you can contact your GP Practice to ask for the test.
Why do I need to be tested if I don’t have GDM anymore?
People who have had GDM have up to a 50% higher risk of developing type 2 diabetes over the next 5 years. You don’t always have symptoms of high blood glucose levels, so checking every year helps to catch any increase early.
I’d like to lose weight or reduce my risk of type 2 diabetes – who can I talk to?
A member of the Diabetes Prevention Team will call you at around 20-24 weeks after you have your baby. We’ll ask how you are getting on and if you feel you would like any support with maintaining lifestyle changes you made during pregnancy. We can offer support to make lifestyle changes which fit in with family life and your new baby. Most importantly though, it’s just a chat to see how you are getting on. If you feel you would like to chat with us earlier or later than our planned call, please get in touch with us at the following email address: fv.diabetespreventionteam@nhs.scot
Diabetes Education, Information and support
- Control It and Diabetes Explained, options for both pre-diabetes and type 2 diabetes – NHS Forth Valley – Type 2 Diabetes
- Diabetes UK
- British Dietetic Association Food Fact Sheets
Other lifestyle support
- Weight Management – here you can access information and tools to self-manage your weight, or self-refer to NHS Forth Valley – Weight Management
- Physical Activity in Forth Valley, including free activity, visit NHS Forth Valley – Physical Activity
- Parent Club tips and advice you can trust about the highs and lows of parenting.
- The Breastfeeding Network local breastfeeding suppport.
Exercise Referral Scheme – local support to be more active at a reduced cost:
First Steps Nutrition– safe and reliable information about nutrition up to age 5
Emotional Wellbeing
- Online mental health support for emotional health, worry, anxiety & stress is available at Online Therapy and CBT
- A range of self help resources for physical and mental wellbeing, including anxiety, bereavement, depression, post natal depression, sleep problems, stress and trauma is available at NHS Forth Valley – Self-Help Resources
- British Dietetic Association fact sheet on Breastfeeding
For Dads
- Dads Rock Provides Dads and families with the tools they need to give their child the best possible start in life.